The hypotensive oedematous septic patient
Albumin
L Gattinoni - likes his albumin
References
Vasopressors
P Marik
Paul Marik giving a long list of what fluids do in sepsis (not good things). Do we want to give water (because we’re giving so much more) or want better cardiac physiology. So, use vasopressors…
Sepsis is a vasodilatory state, not a hypovolemic one - it actually causes vasodilation and increase risk of shock, cardiac dysfunction, and mortality
CVP < 8; above that increase risk of death
Early administration of Norepinephrine increases cardiac preload and cardiac output in septic patients with life-threatening hypotension
- Increased stress volume improves venous return
Norepinephrine is the best study
Vasopressin does not increase mortality, but may reduce Norepinephrine doses
Angiotensin II vs Placebo - does not improve mortality but increases SOFA score
Vitamin C + Thiamine + Hydrocortisone: controversial but data looks extremely promising (rapid deescalation of vasopressor doses, very low mortality, low ICU LOS ~3 day)
Fluid challenges
X Monnet
Notes/Discussions
Confirms that positive fluid balances are detrimental to survival/recovery
Challenge the Frank-Starling curve with fluid challenges
500 mL-1 L crystalloid, 300-500 mL colloids based on SSG
- Day 1: 4-5 fluid challenges = 2 L volume overload with no improvement in CO
French mini-fluid study (100 mL boluses): must be detected with dynamic measurements (echo/VTI)
- Least significant change is 15% (two operators), 10% (single operator)
1-4 mL/kg boluses over 5 min → only able to see effect at 320 mL
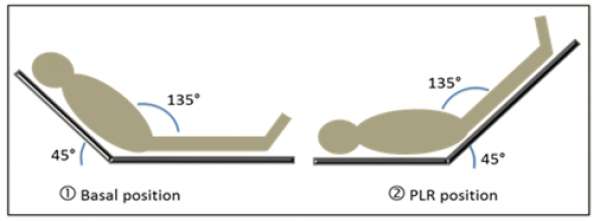
Passive Leg Raising: is it a preload challenge rather than a fluid challenge?
- Potent preload challenge! How much fluid? ~300 mL to obtain same result when given as extraneous fluid
References
Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis.
Commentary by @concernecus
Gattinoni, Marik, and Monnet spent the first part of the afternoon exploring the complicated management of that nightmare scenario: the hypotensive, edematous septic patient. As expected, Gattinoni spoke to us about the use of Albumin and some of the secondary outcomes of the ALBIOS trial, including improved hemodynamics with better fluid balance in those with existing hypoalbuminemia - unfortunately it didn’t offer any mortality benefit, so the debate rages on…
http://www.nejm.org/doi/full/10.1056/NEJMoa1305727#t=article
Marik followed up echoing his long-held sentiment that sepsis is a vasodilated and not a hypovolemic state; therefore it should be treated primarily with Norepinephrine to improve stress venous volume, increase preload, and improve hemodynamics. And then out came the very controversial Vit C/Thiamine/Hydrocortisone recommendations. Dr. Marik referenced some remarkable data, including zero mortality and a rapid de-escalation of vasopressor support when applied early. Thankfully, a randomized controlled study is on the way, so cross your fingers. Is a magic bullet around the corner?
http://journal.chestnet.org/article/S0012-3692(16)62564-3/fulltext
Finally, Dr. Xavier Monnet showed us the data on the detrimental effects of positive fluid balance in critically ill patients and led us along the Frank-Starling Curve to try and discover the “volume responsiveness” pot of gold. The current SSG recommends 0.5-1 L fluid boluses, which routinely leads to a +2 L balance in the first day with no significant improvement in cardiac output. We reviewed the limitations of static and dynamic measurements and ultimately were shown the advantages of the passive leg raise (a ~300 mL “preload” challenge rather than an exogenous fluid one.
https://ccforum.biomedcentral.com/articles/10.1186/s13054-014-0708-5